

Good nights for better days: Why our sleep quality holds the key to our resilience.
Good nights for better days:
Why our sleep quality holds the key to our resilience.
BY: DR. MERET CEPERO MALO | January 20, 2024
Whether it resulted from a lively party, a late-night study session, the demands of caring for a newborn, or the pressures of stress – we ‘ve all experienced the aftermath of a night with insufficient sleep. Facing the day while feeling groggy, hungry, and irritable can seem overwhelming and sometimes, downright impossible. Amid our hectic lives, a good night’s sleep is often the first sacrifice we make to meet a deadline or complete an important task. It’s easy to dismiss a few lost hours of shut-eye, not fully recognizing the toll it takes on our bodies1. However, sleep isn’t just a small piece in the health puzzle; it’s the central pillar of our overall well-being2.
The significance of sleep becomes most evident when we consider that even minimal sleep deprivation can plunge us into unmanageable states and increase our risk for health complications1. Take daylight savings time, for example: each spring when the clock jumps forward by an hour, there is a noticeable increase in fatal traffic accidents3, workplace injuries4, and even heart-attacks5 in the days after the shift. In their 9-week Resilience Training for Researchers, Dr. Nadine Sinclair and Paul Sinclair from Mind Matters explore the critical biological role of sleep in promoting our physical and mental health. In the following blog post, we will shed light on the importance of sleep, as it influences our ability to navigate daily challenges and maintain resilience in the face of adversity.
Why do we need sleep?
The paradoxical nature of sleep is concisely captured in the words of sleep research pioneer Prof. Emeritus Allan Rechtschaffen: “If sleep does not serve an absolutely vital function, then it is the biggest mistake evolution has ever made.” Indeed, considering that sleep immerses us in an altered state of consciousness, rendering us completely incapable of responding to the external world, finding nourishment, or seeking shelter, it’s quite puzzling that humans spend around one third of their lives asleep. The question “Why do we sleep?” has kept researchers and study participants awake for far longer than they wanted to be. In fact, the record for the longest scientifically supervised period without sleep was established in 1964, by 17-year-old high schooler Randy Gardner, who stayed awake for 11 days and 25 minutes as part of a science fair project6. Since then, sleep has remained an active topic of scientific investigation and is often described as “one of the last great biological mysteries”2. Contradicting this sentiment, sleep scientist Professor Russel G. Foster recently published an article titled “There is no mystery to sleep.”7, asking his readers to zoom out and re-examine sleep through the same evolutionary lens that made it so puzzling in the first place. Given that the earth has been rotating upon its axis for 4.54 billion years, causing the cycle of alternating light and dark periods that we know as day and night, it is unsurprising that all forms of life have adjusted to our 24-hour world in one way or another. Thus, sleep might actually represent one of evolution’s greatest adaptations – allowing organisms to conserve energy during resting periods and optimize the performance of vital biological activities to their periods of wakefulness7,8. After exploring our evolutionary need for sleep, let’s dive into the biology of sleep and how it comes about.
The Neurobiological Architecture of Sleep.
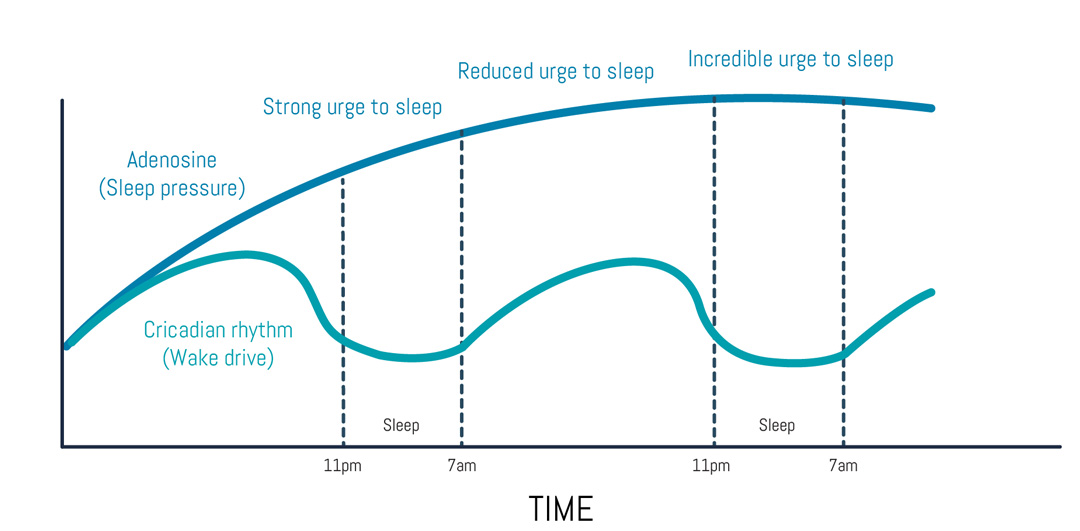
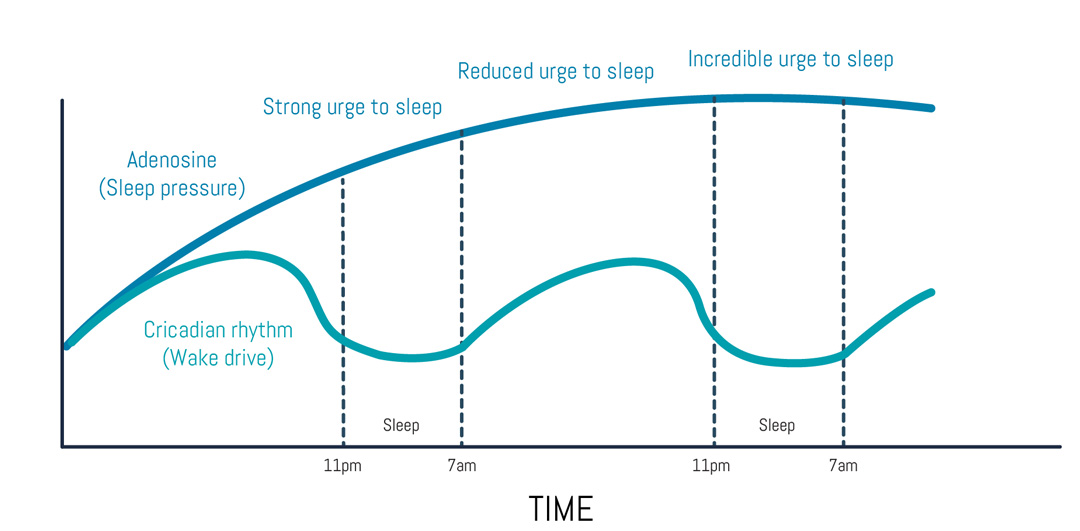
There’s a clock inside your head. Not a literal clock, of course, but a biological one. You can imagine the suprachiasmatic nucleus (SCN), a tiny brain structure located in the anterior part of your hypothalamus, as the pacemaker of your circadian rhythm. Derived from the Latin words “circa” (about) and “dies” (day), our circadian rhythm describes the natural process that regulates the sleep-wake cycle and repeats roughly every 24 hours. Even though our circadian rhythms are generated by our internal clock, they can be synchronized to the state of the outside world via external signals (or zeitgebers) such as light or temperature9. This mechanism allows us respond to disruptions in our circadian rhythm (i.e. shift work or jet lag). By recalibrating to local zeitgebers, our circadian rhythm ensures the alignment of our daytime and nighttime physiology with the current day/night schedule1. In humans, the absence or presence of light from our environment seems to have the biggest influence on our sleep-wake-cycles10. While darkness causes the pineal gland to release melatonin (a hormone that promotes sleepiness11), light exposure (especially in the morning) inhibits the release of melatonin10. During periods of wakefulness, the neuromodulator adenosine gradually builds up in the brain. The binding of adenosine to its A1 and A2A receptors inhibits the release of stimulating neurotransmitters like dopamine and norepinephrine – this, in turn, promotes a state of drowsiness that scientists call “sleep pressure”12. Interestingly, caffeine works by blocking the A2A adenosine receptors13 and temporarily rescuing us from detecting the adenosine build-up in our system – once the caffeine wears off, however, the sleep pressure usually comes crashing down on us and it’s time for a (prolonged) nap2.
Cycling through phases.
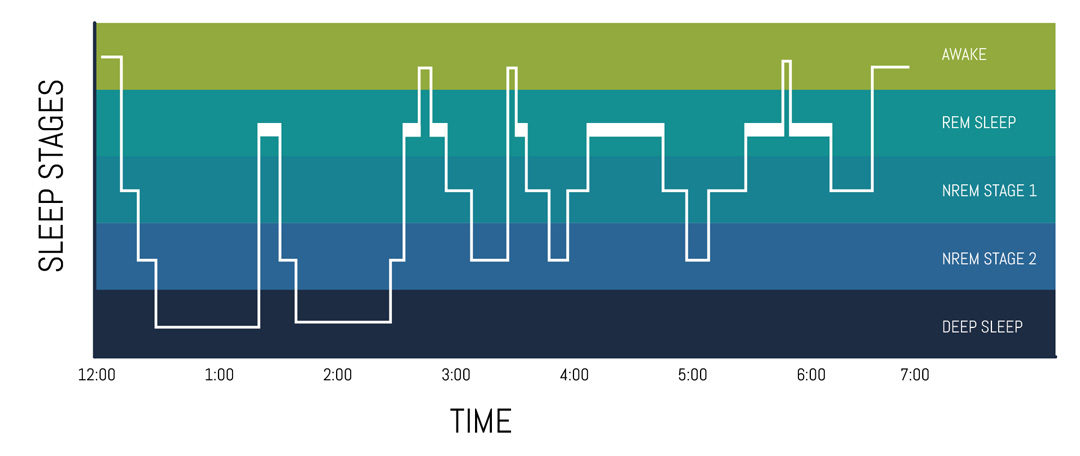
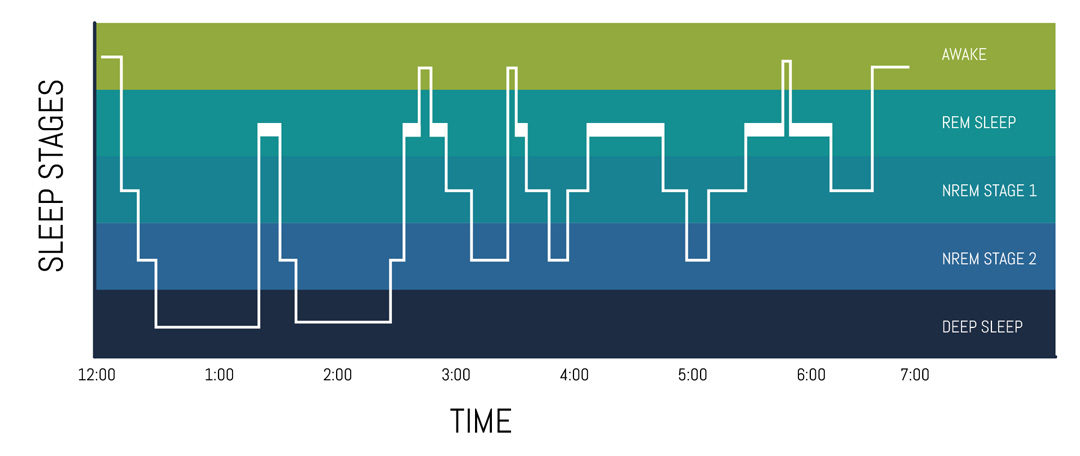
In 1957, sleep researchers Dement and Kleitman used electroencephalographic (EEG) recordings to trace patterns in the electrical brain activity of their participants and discovered that there are two main phases of sleep: non-rapid eye movement (NREM) and rapid eye movement (REM) sleep14. Since their discovery, NREM sleep has been further divided into three stages (N1 to N3), which represent increasing levels of sleep depth and hold unique characteristics in brain wave patterns and muscle tone15. While NREM sleep is largely dreamless, REM sleep constitutes a more active period, during which most dreams occur16. During REM sleep, parts of our brain stem (pons and medulla) send inhibitory signals to our muscles via motor neurons in the spinal cord17, creating a temporary state of full-body paralysis that is designed to prevent us from acting out our dreams18. A full 90-minute sleep cycle is composed of three NREM stages (N1-N3) and a fourth REM sleep stage. Each night, we go through four to six of these sleep cycles18. Importantly, not all sleep cycles are created equal: while the first half of our sleep cycles emphasizes restorative NREM sleep, the second half of a night features more dream-laden REM sleep15. It follows that, besides sleep duration, when we go to bed and when we wake up can also impact our overall sleep health and circadian rhythm2.
Sleep also plays and important role in brain plasticity processes like memory consolidation and learning19. Most notably, so-called sleep spindles, which occur during the slow wave sleep of the NREM stage, seem to aid with the restructuring of neural memory traces, as well as with memory retention20. Finally, it has also been shown that during deep sleep, the brain’s glymphatic system (a “waste-clearance system” formed by astroglial cells) helps to flush out toxins that build up during waking hours21. In sum, adequate sleep is pivotal for the neurobiological maintenance of brain tissue, as well as for cognitive functions such as learning, problem-solving, and creativity.
Sleep & The Body
The universal and essential need for sleep is best illustrated by the detrimental effects that short-term and chronic sleep deprivation can have on our systems. Indeed, studies on sleep deprivation have consistently shown that a lack of sleep is linked to conditions such as obesity, diabetes, cardiovascular diseases, and a decline in mental health1. While sleep is sometimes described as ‘of the brain, by the brain and for the brain’ 22, many of its knock-on effects affect the whole body.
When it comes to physical health and recovery, our body releases beneficial factors like growth hormones during slow wave sleep in early stages of the night – these growth hormones support fat burning, bone building and muscle repair 1,23. Other hormones, such as cortisol (a biomarker for stress levels) are also finely balanced during sleep – cortisol levels rise in the middle of the night and reach their peak just as we wake, to increase our alertness in the morning1,24. Chronic sleep deprivation can impede these fine-tuning processes and has been linked to elevated cortisol levels24. Additionally, substandard sleep has been shown to cause increased hunger25 and a preference for high-carb foods26 – this likely results short nights causing elevated levels of the hunger-promoting hormone ghrelin27 and changes in insulin sensitivity28.
Importantly, our immune system can also be affected by a lack of sleep: sufficient sleep enhances the production of immune cells and antibodies during deep sleep stages, contributing to a robust immune response – when we don’t sleep enough, inflammatory signals (i.e. cytokines) can a rise and leave us more susceptible to illness25,29. Lastly, our emotional resilience also seems to depend on the quality of our sleep – this effect can be looped back to cytokine fine-tuning (or lack thereof during a short night). Increased levels of inflammatory cytokines are linked to an overactive HPA-axis and ever-climbing cortisol levels, making stress management increasingly difficult 1,30. Several studies have highlighted the bidirectional relationship between poor sleep and an increased risk for anxiety and depression 25,31.
Lullabies and Lulla”byes” – The Do’s and Don’ts of a science-based nighttime routine.
After learning that sleep can affect nearly every parameter of our physical and emotional well-being, let’s circle back to the Mind Matters workshop on sleep and apply some of the principles discussed during the session. Given that sleep deprivation is far from uncommon amongst researchers, Nadine and Paul presented four metrics that participants could tweak to improve their sleep in the long run: sleep regularity, sleep efficiency, sleep debt and sleep quality. Lastly, Nadine and Paul introduced a technique called “the bedroom audit”, which invited participants to take a closer look at their sleeping environments and assess the light, sound, temperature, and air quality in their rooms – factors that likely affect their sleep quality during the night. If you want to change your sleep efficiency for the better, but haven’t had a chance to visit the sleep workshop, yet – here are a few “dos and don’ts” that you can consider for your nighttime routine:


By incorporating these science-based practices into your nightly routine, you pave the way for a more restful and refreshing sleep. Remember, a good night’s sleep sets the stage for a better day tomorrow. Lastly, if sleep troubles persist or you find yourself unusually fatigued during the day, don’t hesitate to seek professional advice. Consulting with a healthcare provider can uncover potential sleep disorders, most of which can be effectively treated with the right guidance.
As I put the finishing touches on this blogpost, I notice my eyelids feeling heavier and my yawning becoming more frequent – wait, aren’t these signs of adenosine building up in my brain? Knowing what I know now, about the intricacies of sleep and how it affects our physical health and emotional well-being, I allow the yawning and gently close my laptop.
Time to go to bed…
References:
1. Feingold, C. L. & Smiley, A. Healthy Sleep Every Day Keeps the Doctor Away. Int. J. Environ. Res. Public Health 19, (2022).
2. Walker, M. Why We Sleep: Unlocking the Power of Sleep and Dreams. (Scribner, 2017).
3. Prats-Uribe, A., Tobías, A. & Prieto-Alhambra, D. Excess Risk of Fatal Road Traffic Accidents on the Day of Daylight Saving Time Change. Epidemiology 29, E44–E45 (2018).
4. Barnes, C. M. & Wagner, D. T. Changing to Daylight Saving Time Cuts Into Sleep and Increases Workplace Injuries. J. Appl. Psychol. 94, 1305–1317 (2009).
5. Janszky, I. et al.Daylight saving time shifts and incidence of acute myocardial infarction – Swedish Register of Information and Knowledge About Swedish Heart Intensive Care Admissions (RIKS-HIA). Sleep Med. 13, 237–242 (2012).
6. Gulevich, G., Dement, W. & Johnson, L. Psychiatric and EEG Observations on a Case of Prolonged (264 Hours) Wakefulness. Arch. Gen. Psychiatry 15, 29–35 (1966).
7. Foster, R. G. There is no mystery to sleep. PsyCh J. 7, 206–208 (2018).
8. Freiberg, A. S. Why we sleep: A hypothesis for an ultimate or evolutionary origin for sleep and other physiological rhythms. J. Circadian Rhythms 18, 1–5 (2020).
9. Foster, R. G. Sleep, circadian rhythms and health. Interface Focus 10, (2020).
10. Blume, C., Garbazza, C. & Spitschan, M. Effects of light on human circadian rhythms, sleep and mood. Somnologie 23, 147–156 (2019).
11. Cajochen, C., Kräuchi, K. & Wirz-Justice, A. Role of melatonin in the regulation of human circadian rhythms and sleep. J. Neuroendocrinol.15, 432–437 (2003).
12. Huang, Z.-L., Yoshihiro, U. & Hayaishi, O. The Role of Adenosine in the Regulation of Sleep. Curr. Top. Med. Chem. 11, 1047–1057 (2011).
13. Huang, Z. L. et al.Adenosine A2A, but not A1, receptors mediate the arousal effect of caffeine. Nat. Neurosci. 8, 858–859 (2005).
14. Dement, W. & Kleitman, N. The relation of eye movements during sleep to dream activity: An objective method for the study of dreaming. J. Exp. Psychol. 53, 339–346 (1957).
15. Memar, P. & Faradji, F. A Novel Multi-Class EEG-Based Sleep Stage Classification System. IEEE Trans. Neural Syst. Rehabil. Eng. 26, 84–95 (2018).
16. Tarun, A. et al.NREM sleep stages specifically alter dynamical integration of large-scale brain networks. iScience 24, 101923 (2021).
17. Jalal, B. & Ramachandran, V. S. Sleep paralysis, “The ghostly bedroom intruder” and out-of-body experiences: The role of mirror neurons. Front. Hum. Neurosci. 11, 2015–2017 (2017).
18. Hobson, J. A. & Friston, K. J. Waking and dreaming consciousness: Neurobiological and functional considerations. Prog. Neurobiol. 98, 82–98 (2012).
19. Davidson, P. & Pace-Schott, E. The role of sleep in fear learning and memory. Curr. Opin. Psychol. 34, 32–36 (2020).
20. Cowan, E. et al.Sleep spindles promote the restructuring of memory representations in ventromedial prefrontal cortex through enhanced hippocampal–cortical functional connectivity. J. Neurosci. 40, 1909–1919 (2020).
21. Jessen, N., Finmann Munk, A. S., Lundgaard, I. & Nedergaard, M. The Glymphatic System – A Beginner’s Guide. Neurochem Res. 40, 2583–2599 (2015).
22. Hobson, J. A. Sleep is of the brain, by the brain and for the brain. Nature 437, 1254–1256 (2005).
23. Hopfinger, A. J. Human Growth Hormone Release : Sleep-Waking Cycles. Science (80-. ).513–516 (1969).
24. Gamble, K. L., Berry, R., Frank, S. J. & Young, M. E. Circadian clock control of endocrine factors. Nat. Rev. Endocrinol. 10, 466–475 (2014).
25. Rihm, J. S. et al.Sleep deprivation selectively upregulates an amygdala–hypothalamic circuit involved in food reward. J. Neurosci. 39, 888–899 (2019).
26. Nedeltcheva, A. V. et al.Sleep curtailment is accompanied by increased intake of calories from snacks. Am. J. Clin. Nutr. 89, 126–133 (2009).
27. Taheri, S., Lin, L., Austin, D., Young, T. & Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 1, 210–217 (2004).
28. Donga, E. et al.A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J. Clin. Endocrinol. Metab. 95, 2963–2968 (2010).
29. Shearer, W. T. et al.Soluble TNF-αreceptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J. Allergy Clin. Immunol. 107, 165–170 (2001).
30. Irwin, M. R. et al.Sleep Loss Activates Cellular Inflammatory Signaling. Biol. Psychiatry 64, 538–540 (2008).
31. Bastos, L. M. V. et al.Sleep loss causes emotional dysregulations increasing depression and anxiety: a reciprocal relationship. Brazilian J. Heal. Rev. 6, 16367–16382 (2023).
Related post
Building Resilience: What 9 weeks taught me about responding, rather than reacting
The Power of saying “no”: Building stronger relationships with Boundaries
A cup half full: how a positive outlook can fuel perseverance


Dr. Meret Cepero Malo
Dr. Meret Cepero Malo is a writer turned neuroscientist, or a neuroscientist turned writer. While pursuing her Ph.D. in Cellular Neuroscience, she participated in ‘Fast Forward’, a 7-week project management course for researchers, eventually taking on a recurring tutoring role. Now, she has teamed up with Dr. Nadine Sinclair and Paul Sinclair from Mind Matters to offer readers a personal account of her experiences in the 9-week Resilience Training. Get ready to be captivated by her storytelling as she delves into the neurobiological foundations of resilience and shares actionable tips for readers on their own resilience journey.






